Overview
Achilles tendinitis is an injury of the Achilles (uh-KILL-eez) tendon. It can be caused by using it too much or too hard without enough rest, called overuse. Or it can develop without a clear cause. The Achilles tendon is the band of tissue that joins calf muscles at the back of the lower leg to the heel bone.
Achilles tendinitis also is called Achilles tendinopathy. It often occurs in runners who have suddenly increased how hard or long they run. It's also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends.
Most often, Achilles tendinitis can be treated with at-home care guided by a healthcare professional. Self-care steps can be helpful to prevent Achilles tendinitis from returning.
Serious cases of Achilles tendinitis can lead to tendon tears, also called ruptures. Tears might need surgery to fix them.
Symptoms
Achilles tendinitis pain most often begins as a mild ache in the back of the leg or above the heel after running or other sports activity. More-severe burning or aching pain might occur after running a long time, stair climbing or sprinting. Over time, there might be pain even at rest.
Achilles tendinitis can make it hard to use the affected foot. The area also might be tender or stiff, especially in the morning. The soreness usually gets better with mild activity.

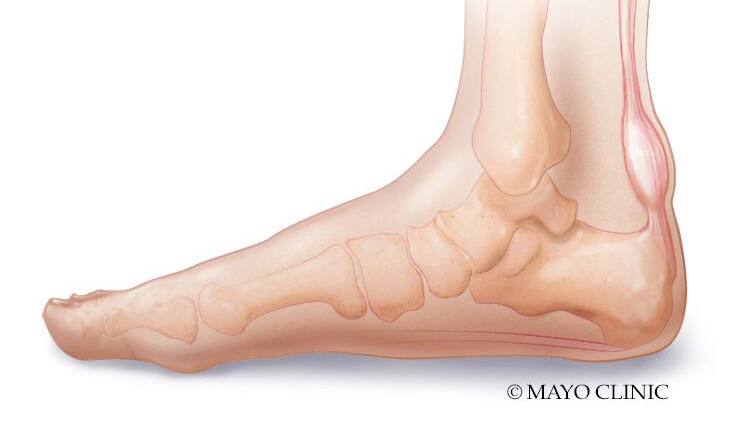
Achilles tendinitis
Achilles tendinitis is an injury of the Achilles (uh-KILL-eez) tendon often caused by too much use. The Achilles tendon is the band of tissue that joins calf muscles at the back of the lower leg to the heel bone.
When to see a doctor
If you have pain around the Achilles tendon that doesn't go away, call your healthcare professional. If the pain is suddenly severe or keeps you from moving, you may have torn your Achilles tendon. Seek medical help right away.
From Mayo Clinic to your inbox
Causes
Repeated or intense strain on the Achilles tendon can cause Achilles tendinitis, though sometimes the cause is not clear. The Achilles tendon is the band of tissue that joins the calf muscles to the heel bone. This tendon is used while walking, running, jumping, climbing or standing on tip toes. Achilles tendinitis can occur within the middle part of the tendon or where it attaches to the heel bone.
The Achilles tendon weakens with age. That can make it easier to injure. This is true for people who play sports only on the weekends or who start running farther, faster or longer without building up over time.
Risk factors
Factors that can raise the risk of Achilles tendinitis include:
- Age. Achilles tendinitis is more common with age.
- Physical problems. A flat arch in the foot or a high arch can increase strain in the Achilles tendon. Obesity and tight calf muscles also can increase tendon stress. Having legs that are different lengths also can increase the risk.
- Having had Achilles tendinitis. This increases the risk of getting it again.
- Training choices. Running in worn-out shoes can increase the risk of Achilles tendinitis. So can running with poor form. Tendon pain occurs more often in cold weather than in warm weather. Running hills also can raise the risk of Achilles injury.
- Medical conditions. People who have the skin condition called psoriasis, high cholesterol or high blood pressure are at higher risk of getting Achilles tendinitis.
- Medicines. Certain types of antibiotics, called fluoroquinolones, have been linked with higher rates of Achilles tendinitis.
Complications
Achilles tendinitis can weaken the tendon. The weakness makes it more likely to tear, also called rupture. An Achilles rupture is a serious injury that often needs surgery to repair it.
Prevention
It may not be possible to prevent Achilles tendinitis. But here are some ways to reduce the risk:
- Increase your activity level slowly. If you're just starting a new exercise, start slowly. Increase how long and hard you train little by little.
- Take it easy. Do not do activities that put a lot of stress on your tendons, such as hill running, if you're not used to them. If you do a hard activity, warm up first by exercising at a slower pace. If you notice pain during an exercise, stop and rest.
- Choose your shoes well. The shoes you wear for exercise should cushion your heel. They should have a firm arch support to help reduce the tension in the Achilles tendon. Replace worn-out shoes. If your shoes are in good shape but don't support your feet, try arch supports in both shoes.
- Stretch daily. Take the time to stretch your calf muscles and Achilles tendon in the morning and before and after exercise. This is to keep the tendon flexible. It also can keep Achilles tendinitis from happening again.
- Strengthen your calf muscles. Strong calf muscles help the calf and Achilles tendon handle the stresses of exercise.
- Cross-train. Do not do high-impact activities, such as running and jumping, every day. On off-days, do low-impact activities, such as cycling and swimming.